During the COVID-19 pandemic, Montana Medicaid wasn’t processing redeterminations or renewing member eligibility for coverage. Soon, Montana Medicaid will start to process redeterminations and will be reaching out to Medicaid and HMK members through the mail.
Follow the steps below to prevent a gap in your Medicaid and HMK coverage while Montana Medicaid is working through the redetermination process.
1. UPDATE YOUR CONTACT INFORMATION
Make sure Montana Medicaid has your current mailing address, phone number, email, or other contact information. This way they will be able to contact you about your Medicaid or HMK coverage. Click on this link to access the contact information online form DPHHS (accessgov.com).Forms can be returned by any of the following methods:
- Submit the form online;
- OR mail it to:
- DPHHS
- PO BOX 202925
- Helena, MT 59620-2925;
- OR fax to 1-877-418-4533;
- OR by stop by Greater Valley Health Center to complete your address change form;
- OR visit any Office of Public Assistance field offices.

2. LOOK AT THE LIMITS AND START WINDOW SHOPPING
In order to continue to qualify for Montana Medicaid, you must meet the monthly income guidelines provided below.
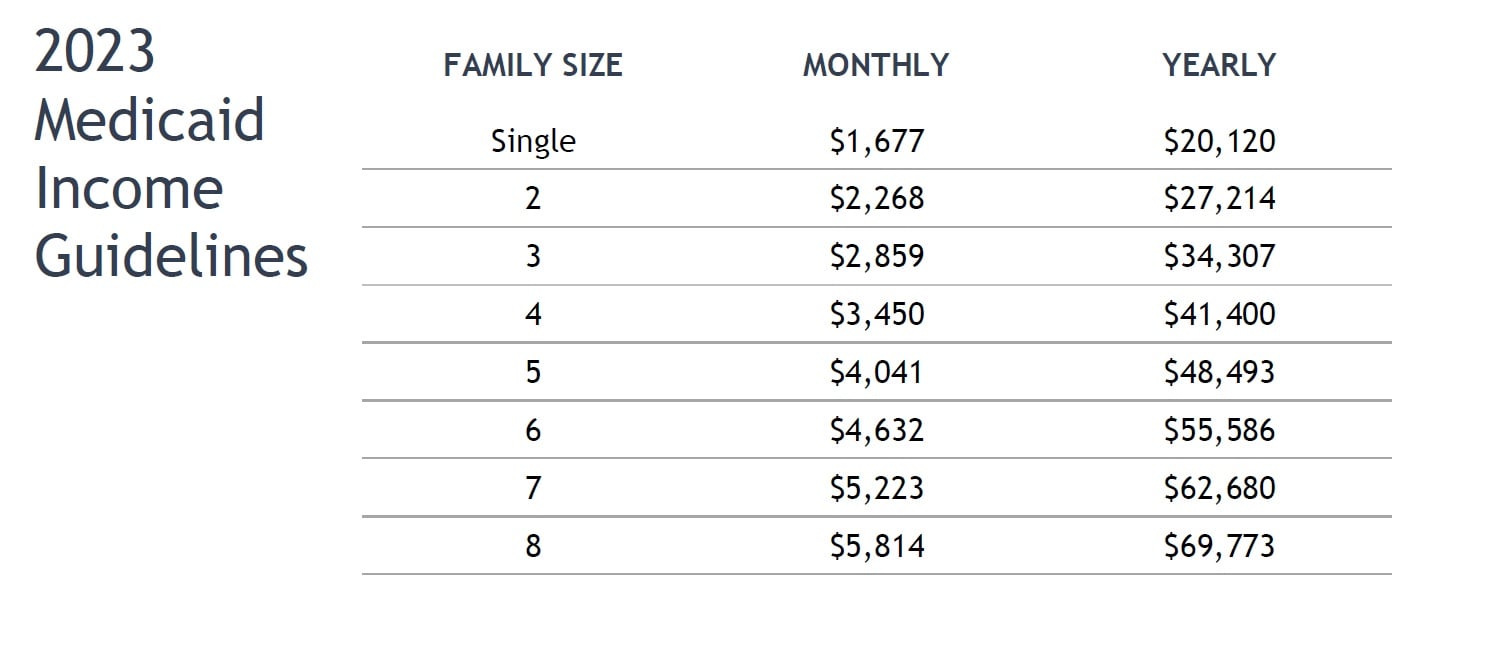

If you feel like you no longer qualify to keep your Medicaid benefits based in the income guidelines, you may be able to buy a health plan through the Health Insurance Marketplace. Marketplace plans are affordable and comprehensive. Four out of five people can find plans that cost less than $10 per month. Most plans cover things like prescription drugs, doctor visits, urgent care, hospital visits, and more. Our staff at Greater Valley Health Center can help you with other options for health insurance. Contact one of our Certified Application Counselors at 406-607-4886 to set up an appointment to review your options before you lose your Medicaid coverage.
3. CHECK YOUR MAIL AND RESPOND TO MEDICAID

Keep an eye on your mailbox. Montana Medicaid will mail you a letter about your Medicaid or CHIP coverage. This letter will let you know if you need to complete a renewal form to see if you still qualify for Medicaid. If you get a renewal form, fill it out and return it to Montana Medicaid right away; you only have 60 days to respond. If you have questions, Greater Valley Health Center’s Certified Application Counselors can help you through this process
4. CONTACT GVHC
Greater Valley Health Center has Certified Application Counselors who can help you work through the renewal process with Medicaid or help you to find coverage through the Marketplace if you no longer qualify for Medicaid or CHIP benefits.
Call 406-607-4886.
